BLOG

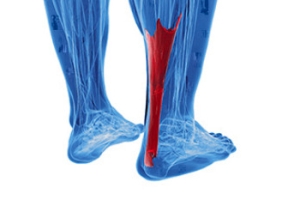
Achilles Tendon Bursitis
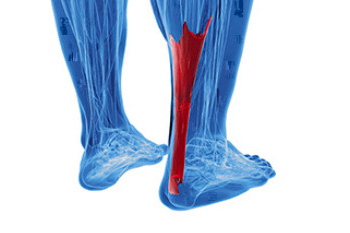
Achilles tendon bursitis is a painful condition that involves inflammation of the fluid filled sac, or bursa, located between the skin of the heel. Posterior Achilles tendon bursitis affects the back of the heel, while anterior Achilles tendon bursitis, also called retromalleolar bursitis, is felt in front of the attachment of the Achilles tendon to the heel bone. Symptoms include swelling, warmth, pain, and a tender spot at the back of the heel. Diagnosis by a podiatrist begins with a discussion of symptoms and a medical history, followed by a physical examination to identify signs of inflammation and tenderness. X-rays may be used to rule out other potential causes of heel pain, and in some cases, an ultrasound or MRI may provide more detailed views. The primary goal is to relieve inflammation and reduce pain. Treatment approaches may vary based on the severity and location of the pain. In rare cases, surgical intervention may be considered. For help in relieving the pain of Achilles tendon bursitis, it is suggested that you make an appointment with a podiatrist.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of Livingston Foot Care Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in North Bellmore, NY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
What are Achilles Tendon Injuries
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
Fungal and Bacterial Infections From Wearing Flip-Flops

Wearing flip-flops leaves your feet vulnerable to various infections, from bacteria to viruses. When your feet are exposed in public places, harmful organisms, such as staphylococcus, can cling to them. This bacterium can cause skin irritation, and in extreme cases, serious foot conditions may emerge. The risk increases if you have open sores or even small wounds from recent pedicures. Another concern is athlete's foot, which is a contagious fungal infection that causes itching. Walking with minimal footwear increases the chances of encountering and contracting this fungus. You also risk exposure to the virus responsible for warts, which is HPV, while wearing flip-flops. If you enjoy wearing flip-flops, it is suggested that you make an appointment with a podiatrist to discuss similarly easy and comfortable footwear alternatives that are healthier for your feet.
Flip-flops can cause a lot of problems for your feet. If you have any concerns about your feet or ankles, contact one of our podiatrists from Livingston Foot Care Specialists. Our doctors will assist you with all of your foot and ankle needs.
Flip-Flops and Feet
Flip-flops have managed to become a summer essential for a lot of people. While the shoes may be stylish and easy to slip on and off, they can be dangerous to those who wear them too often. These shoes might protect you from fungal infections such as athlete’s foot, but they can also give you foot pain and sprained ankles if you trip while wearing them.
When Are They Okay to Wear?
Flip-flops should only be worn for very short periods of time. They can help protect your feet in places that are crawling with fungi, such as gym locker rooms. Athlete’s foot and plantar warts are two common fungi that flip-flops may help protect your feet against.
Why Are They Bad for My Feet?
These shoes do not offer any arch support, so they are not ideal for everyday use. They also do not provide shock absorption or heel cushioning which can be problematic for your feet. Additionally, you may suffer from glass cuts, puncture wounds, and stubbed toes since they offer little protection for your feet.
More Reasons Why They Are Bad for Your Feet
- They Slow You Down
- May Cause Blisters and Calluses
- Expose Your Feet to Bacteria
If you have any questions, please feel free to contact our office located in North Bellmore, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Flipping Out About Flip Flops
Although it may be tempting to wear flip-flops in warm weather, they are not the best choice of footwear for your feet. Flip-flops may be ideal for the beach, pool, spa, and shared showers, but you should avoid wearing them unless it is completely necessary.
Flip-flops only have a small strip of fabric holding your foot in place, but your toes need a better grip to keep your foot in place. The repetitive gripping can lead to an overuse of your muscles, which could result in tendinitis. This is only one of the many problems that stem from wearing flip-flops too often.
Flip flops aren’t good for extensive walking because they fail to offer arch support, heel cushioning, or shock absorption. As a result, people who wear flip flops are at a higher risk of experiencing an ankle sprain. Additionally, these shoes offer little protection for your feet, putting those who wear them at a greater risk for stubbed toes, glass cuts, and puncture wounds.
Although flip flops aren’t recommended for everyday use by anyone, it is especially important for diabetics to avoid them. A diabetic foot injury can easily become very serious, and it may even lead to amputation.
If you are experiencing pain from wearing flip-flops, you shouldn’t be hesitant to replace them with a more comfortable shoe that offers more support. If your flip-flop foot pain doesn’t go away, you should seek assistance from a podiatrist right away. It is possible that you may have a more serious foot problem such as a stress fracture or arthritis.
Treatment for Broken Ankles

Broken ankles, also known as ankle fractures, can vary from minor hairline fractures to severe, multiple fractures. They occur when one or more of the bones that make up the ankle joint are broken. The type of fracture often determines the treatment needed. Simple fractures may need immobilization with a cast or splint to ensure proper alignment during healing. More complex fractures, particularly those where the bones are out of place or the ankle joint is unstable, may require surgery. The surgical intervention aims to realign the bones and secure them in place with screws, plates, or pins. During post-surgery, the ankle is generally immobilized, and weight-bearing may be restricted for a certain period. If you have broken your ankle, it is strongly suggested that you make an appointment with a podiatrist for a proper diagnosis and prompt treatment to reduce the risk of complications.
Broken ankles need immediate treatment. If you are seeking treatment, contact one of our podiatrists from Livingston Foot Care Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
Broken Ankles
A broken ankle is experienced when a person fractures their tibia or fibula in the lower leg and ankle area. Both of these bones are attached at the bottom of the leg and combine to form what we know to be our ankle.
When a physician is referring to a break of the ankle, he or she is usually referring to a break in the area where the tibia and fibula are joined to create our ankle joint. Ankles are more prone to fractures because the ankle is an area that suffers a lot of pressure and stress. There are some obvious signs when a person experiences a fractured ankle, and the following symptoms may be present.
Symptoms of a Fractured Ankle
- Excessive pain when the area is touched or when any pressure is placed on the ankle
- Swelling around the area
- Bruising of the area
- Area appears to be deformed
If you suspect an ankle fracture, it is recommended to seek treatment as soon as possible. The sooner you have your podiatrist diagnose the fracture, the quicker you’ll be on the way towards recovery.
If you have any questions, please feel free to contact our office located in North Bellmore, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
All About Broken Ankle
Broken ankles or “ankle fractures” are injuries that occur when the bones that make up the ankle joint are broken. Ankle injuries are some of the most common bone and joint injuries. The ankle joint is made up of three bones that join. The tibia is the main bone, and it makes up the inside of the anklebone. The fibula is a smaller bone, and it makes up the outside of the anklebone. A membrane called the joint capsule is lined with a layer called the synovium, which covers the entire joint. The synovium produces synovial fluid which allows for the joint surfaces to move.
An ankle becomes broken when the joint is stressed beyond the strength of its limits. When an ankle is fractured, ligaments may also tear at the same time. Fractures often occur to the ankle rolling or twisting in an unusual way. At times, a fracture may even be caused by an extreme force applied to the joint.
Symptoms of a broken ankle include pain, swelling, bruising, discoloration, numbness, and an inability to move the toes. If you have a broken ankle, you may also hear something tear or snap when you initially suffered the injury. If you have pain from a broken ankle, beware that the pain will not always come from the exact area of the fracture; you may also experience pain from associated foot fractures. The swelling you may experience can suggest that soft tissue damage may have occurred due to the injury.
There are differences between an ankle fracture and an ankle sprain. The difference is that a fracture or break in the bone is required to classify an injury as a broken ankle. An ankle sprain occurs when there is a tear or disruption of ligaments in the ankle. In some cases, the prognosis of an ankle sprain may be worse than that of a fracture.
X-rays are the most common way to diagnose a broken ankle. X-rays show if the ankle is broken and where exactly the fracture is located. It will also show how many pieces of broken bone there are. A second method of testing to see if an ankle is broken is a stress test. To do this, the doctor will put pressure on the ankle and perform a stress test to determine if the fracture requires surgery. Other methods for diagnosis include CT scans and MRI scans.
If you are suffering from a broken ankle, consult with your podiatrist immediately to receive a proper diagnosis and treatment.
Corns and Calluses on the Feet

Corns and calluses are skin conditions that result from excess pressure or friction on the feet. A common cause of corns and calluses is wearing ill-fitting shoes, particularly high heels. Tight or uncomfortable footwear, not wearing socks with shoes, and engaging in activities that involve repetitive movements, can result in the formation of corns and calluses. If a corn or callus becomes infected, treatment options include taking antibiotics. Symptoms are redness, warmth, swelling, or discharge. In such cases, a podiatrist can prescribe medication to combat the infection. In the case of stubborn corns or calluses, a podiatrist can offer a range of treatments. Included are debridement to remove the hardened skin and adding padding and insoles to redistribute pressure. In certain situations, custom orthotic devices may be prescribed to address structural issues, and topical medications may be applied to soften the affected area. Prevention of corns and calluses on the feet involves wearing properly fitting shoes and addressing any underlying foot problems. If you need help dealing with problematic corns or calluses on the feet, it is suggested that you make an appointment with a podiatrist.
Corns can make walking very painful and should be treated immediately. If you have questions regarding your feet and ankles, contact one of our podiatrists of Livingston Foot Care Specialists. Our doctors will treat your foot and ankle needs.
Corns: What Are They? And How Do You Get Rid of Them?
Corns are thickened areas on the skin that can become painful. They are caused by excessive pressure and friction on the skin. Corns press into the deeper layers of the skin and are usually round in shape.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as:
- Wearing properly fitting shoes that have been measured by a professional
- Wearing shoes that are not sharply pointed or have high heels
- Wearing only shoes that offer support
Treating Corns
Although most corns slowly disappear when the friction or pressure stops, this isn’t always the case. Consult with your podiatrist to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact our office located in North Bellmore, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Understanding Corns and Calluses
Corns and Calluses are both hardened layers of thickened skin that develop because of friction. Both ailments are typically found on the feet and may be unsightly. Although they have similarities, corns and calluses are different from each other.
Some causes of corns and calluses may be wearing ill-fitting shoes and not wearing socks. If you wear tight shoes, your feet will constantly be forced to rub against the shoes, causing friction. If you fail to wear socks, you are also causing your feet to endure excess friction.
There are some signs that may help you determine whether you have one of these two conditions. The first symptom is a thick, rough area of skin. Another common symptom is a hardened, raised bump on the foot. You may also experience tenderness or pain under the skin in addition to flaky, dry, or waxy skin.
There are also risk factors that may make someone more prone to developing corns and calluses. If you are already dealing with bunions or hammertoe, you may be more vulnerable to having corns and calluses as well. Other risk factors are foot deformities such as bone spurs, which can cause constant rubbing inside the shoe.
Corns tend to be smaller than calluses and they usually have a hard center surrounded by inflamed skin. They also tend to develop on the parts of the body that don’t bear as much weight such as the tops and sides of toes. Corns may also be painful for those who have them. On the other hand, calluses are rarely painful. These tend to develop on the bottom of the feet and may vary in size and shape.
Fortunately, most people only need treatment for corns and calluses if they are experiencing discomfort. At home treatments for corns and calluses should be avoided, because they will likely lead to infection. If you have either of these ailments it is advised that you consult with your podiatrist to determine the best treatment option for you.
Suggested Footwear Options for Diabetics

Diabetic foot complications can be debilitating, but choosing the appropriate footwear can help to manage the symptoms. Diabetic shoes are specially designed with extra depth and a roomy toe box to accommodate custom orthotics or insoles. These shoes are typically made from soft, breathable materials to minimize friction and pressure points, as well as reduce the risk of blisters, calluses, and ulcers. Diabetic shoes often feature seamless interiors and come with supportive arches and cushioned insoles for added comfort. Custom orthotics, prescribed by a podiatrist, are designed to provide personalized support for your unique foot structure and gait. These can be placed inside your regular shoes or diabetic shoes, offering stability, shock absorption, and pressure relief where needed. Extra-wide shoes are a good choice, as they offer ample room for the feet without causing pressure or constriction. Shoes with adjustable closures, such as Velcro straps or laces, can provide a secure fit without excessive tightness. Many people choose to wear diabetic socks, which are generally made from moisture-wicking materials to keep your feet dry and comfortable. They typically have seamless construction to minimize friction and reduce the risk of blisters and ulcers. If you have foot conditions caused by diabetes, it is suggested that you are under the care of a podiatrist who can monitor and manage any problems that may occur.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from Livingston Foot Care Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in North Bellmore, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.